Commercially Insured Patients: As little as $0* co-pay
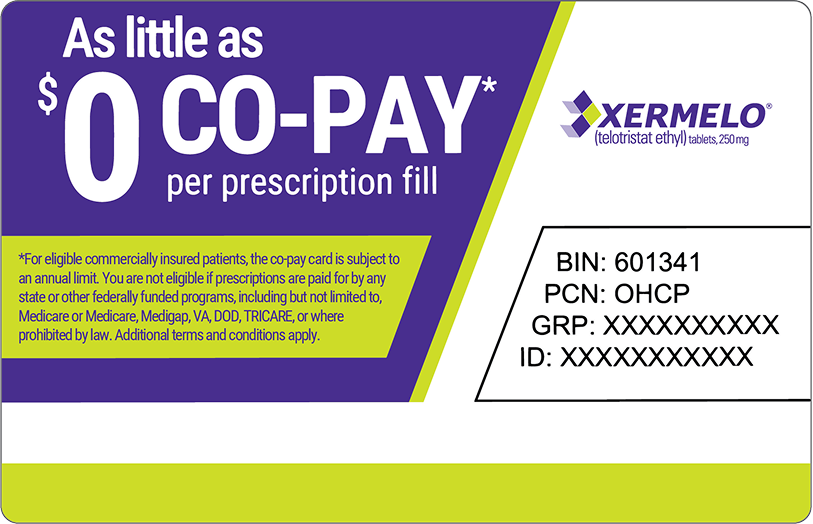
Not actual card.
Please complete the form below to see if you're eligible for the XERMELO Co‑pay Savings Program.
XERMELO Co-pay Savings Program Terms and Conditions
Eligibility Criteria
By enrolling in the XERMELO® (telotristat ethyl) Co-pay Savings Program (the "Program"), you acknowledge that you currently meet the following eligibility criteria, subject to the Terms and Conditions below:
- You are a resident of the United States, the District of Columbia, Puerto Rico, Guam, or the USVI;
- You are lawfully prescribed XERMELO;
- You are at least 18 years of age;
- Your prescription will be used exclusively for you;
- You have commercial insurance that covers XERMELO;
- You are not enrolled in Medicare, Medicaid, Veterans Affairs (VA), the Department of Defense (DoD), or any other state or federal plans; and
- You accept the Program Terms and Conditions.
Specifically, because federal and state laws and other factors may prevent or otherwise restrict eligibility, if you are enrolled in Medicare, Medicaid, Veterans Affairs (VA), the Department of Defense (DoD), or any other state or federal plans, you are not eligible to enroll in the XERMELO Co-pay Savings Program.
Terms and Conditions
The XERMELO Co-pay Card is available to patients with commercial insurance that covers XERMELO, regardless of financial need or the amount of coverage. The Program is not valid for patients that are enrolled in Medicare, Medicaid, Veterans Affairs (VA), the Department of Defense (DoD), or any other state or federal plans. The XERMELO Co-pay Card is not valid for cash-paying patients or where prohibited by law. (See Eligibility Criteria above.)
The XERMELO Co-pay Card may help lower your XERMELO out-of-pocket medication costs. Out-of-pocket costs may include co-payment, co-insurance, and deductible out-of-pocket costs. The XERMELO Co-pay Card does not cover any other costs related to physician office visits or administration of the product. The XERMELO Co-pay Card provides support up to the Maximum Program Benefit or Patient Total Program Benefit. If a patient's commercial insurance plan imposes different or additional requirements on patients who receive XERMELO Co-Pay Card benefits, TerSera has the right to modify or eliminate those benefits. Whether you are eligible to receive the Maximum Program Benefit or Patient Total Program Benefit is determined by the type of plan coverage you have. Please ask your XERMELO Support Case Manager to help you understand eligibility for the XERMELO Co-pay Card, whether your particular insurance coverage is likely to result in your reaching the Maximum Program Benefit or your Patient Total Program Benefit amount by calling 1-844-XERMELO (1-844-937-6356).
XERMELO patients may pay as little as $0 out-of-pocket for each prescription fill, dose, or cycle of XERMELO.
TerSera will pay the remaining eligible out-of-pocket costs on behalf of the patient until the TerSera payments have reached either the Maximum Program Benefit and/or the Patient Total Program Benefit. Patients are responsible for all amounts that exceed this limit.
Maximum Program Benefit, Patient Total Program Benefit, Benefits May Change, End, or Vary Without Notice: The Program provides up to a Maximum Program Benefit of assistance to reduce a patient's out-of-pocket medication costs that TerSera will provide per patient for each calendar year, which must be applied to the patient's out-of-pocket costs (co-pay, deductible, or co-insurance and annual out-of-pocket maximum). Patient Total Program Benefit amounts are unilaterally determined by TerSera in its sole discretion and will not exceed the Maximum Program Benefit. The Patient Total Program Benefit may be less than the Maximum Program Benefit, depending on the terms of a patient's plan, and may vary among individual patients covered by different plans, based on factors determined solely by TerSera, to ensure all Program funds are used for the benefit of the patient. Each patient is responsible for costs above the Patient Total Program Benefit amounts.
Participating patients are solely responsible for updating TerSera with changes to their insurance including, but not limited to, initiation of, or enrollment in, insurance provided by any government healthcare program (including, Medicare, Medicaid, Veterans Affairs [VA], the Department of Defense [DoD]), the addition of any coverage terms that do not apply XERMELO Co-pay Card benefits to reduce a patient's out-of-pocket costs, such as accumulator adjustment benefit design or a co-pay maximization program. Participating patients are responsible for providing TerSera with accurate information necessary to determine Program eligibility. By accepting payments from TerSera made on behalf of participating patients, participating PBMs and Plans likewise are responsible for providing TerSera with accurate information regarding patient eligibility.
Patients may use the XERMELO Co-pay Card every time they receive a XERMELO prescription fill, dose, or cycle, up to the Maximum Program Benefit or Patient Total Program Benefit, which reset each calendar year. Reenrollment in the Program may be required at regular intervals. Patients may continue in the Program as long as the patient re-enrolls as required by TerSera and continue to meet all of the Program's eligibility requirements during participation in the Program.
TerSera may cancel or terminate the XERMELO Co-pay Card at any time without notice or further obligation. In addition, some health plans have established programs referred to as "co-pay maximizer" programs. Co-pay maximizers are programs in which the amount of your out-of-pocket costs is increased to reflect the availability of support offered by a manufacturer assistance program. Since you may be unaware whether you are subject to a co-pay maximizer program when you enroll in the XERMELO Co-pay Savings Program, TerSera will monitor Program utilization data and reserves the right to discontinue co-pay assistance at any time if TerSera determines that you are subject to a co-pay maximizer program.
Please ask your XERMELO Support Case Manager to help you understand eligibility for the XERMELO Co-pay Card by calling 1-844-XERMELO (1-844-937-6356).